Sometimes a tooth breaks, decays, or becomes loose to the extent that it can not be restored and needs to be extracted. It is the standard of care to place a bone grafting in the extraction site where the root of the tooth was, in order to support an implant, partial or full denture, or support the teeth holding a bridge. In addition, wisdom teeth extractions are a fairly common procedure. While we do perform many extractions, wisdom teeth extractions are often referred to an oral surgeon.
Wisdom teeth often cause problems as they are trying to protrude through the gums. When a wisdom tooth is impacted, it means the tooth is coming in at an angle and not straight through the gum line. This can cause pain. The tooth can come in unevenly, or the tooth may only emerge partially.
When a wisdom tooth only emerges partially a flap of skin, called an operculum, may form over the tooth. This can make the tooth hard to clean, and pieces of food may be caught under the skin. This makes it easy for an infection, called pericoronitis, to develop. This often causes swelling and pain in the area.
Impacted teeth and wisdom teeth that can potentially cause problems, like infections, need to be removed. Extractions can range from a single tooth, to removing all four wisdom teeth at once. Based on the preference of the doctor and/or the patient, a local anesthetic could be used to numb the areas where the teeth will be extracted. Others will prefer to go under a general anesthetic so that they will be sedated during the procedure.
The gum tissue around the wisdom tooth is cut open to reveal the tooth. The tooth is loosened by gripping it tightly and wiggling it back and forth until it can be lifted out of the gums. Sometimes a tooth may be impacted so tightly that it cannot be simply lifted out of the gums. In cases like this the tooth will be broken up into pieces first before being removed. Depending on the incision and extraction site, sutures may be needed to close the area.
Post-Op
After the surgery you will need to rest. You need to be driven home by a friend or family member if you go under general anesthesia. You can expect for the extraction site to bleed for a little while after the surgery. Gauze will be applied at the completion of the surgery, and you will need to change it when it becomes soaked. If bleeding continues for longer than 24 hours you should call us. Rest when you return home, but do not lie flat. This could prolong the bleeding. Prop your head up on a pillow when lying down. If we prescribe you pain medication, take as directed. You can also use an ice pack for the pain. On occasion we might also provide you with a cleaning solution to clean the extraction site.
You will be limited to soft foods for a few days after your surgery. Some recommended foods are:
- Gelatin
- Pudding
- Yogurt
- Mashed Potatoes
- Ice Cream
- Thin Soups
- …and other food you can eat without chewing.
When drinking, make sure you do not use a straw. The sucking motion can loosen your sutures and slow the clotting process. The same goes for smoking. If you have prolonged pain, bleeding, irritation, or don’t feel that the extraction site is healing properly call us for a follow up.
Site Preservation
When removing a tooth it is important to consider what will be done with the empty space after that tooth is removed. Wisdom teeth are in the back of the mouth, so that site should heal on its own without complications. If it is necessary to remove another tooth, plans must be made. If a tooth is removed and nothing is done with the extraction site, the jaw bone will degenerate and change shape during healing and can cause your teeth to shift. This can create problems in your bite and affect your ability to speak and chew.
If you want to fill the space with a dental implant, a sturdy jaw bone is necessary to place the implant. If you opt for a dental bridge, the bridge must be molded and placed before the teeth shift.
Your dentist is always open to a conversation on what you would like to do with your extraction site before removing a tooth. They will be able to make a recommendation and layout a treatment plan. Make sure to schedule follow up appointments to properly care for your extraction site.
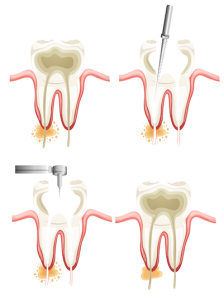
Endodontics is the dental specialty that deals with the nerves of the teeth. Root canals are probably the most notorious procedure in dentistry and the most common procedure relating to endodontics. When a tooth becomes infected it is usually related to the nerves in the root of the tooth. The infected nerves need to be removed. If left untreated an infection can turn into an abscess, which is a much more serious problem that includes bone loss in the jaw.
The area around the tooth is numbed with a local anesthetic to start the procedure. We then drill down into the tooth to create an opening into the canal. Then we are able to remove infected tissue and clean the canal. After the infection has been removed, the space is filled with a sealant called gutta percha. It is highly recommended that a tooth that has undergone a root canal is fitted with a crown right away. This will improve the appearance of the tooth, and will also make it much more likely that the root canal is successful.
“Root canal” has become a scary term for dental patients to hear, but the benefits of the procedure and advances in dental technology have made it much less “scary”. Local anesthetics and proper pain medication allow the procedure to be performed with little to no pain in most cases. There may be some soreness following the procedure, but that is normal for most dental procedures. Over the counter painkillers are usually enough to relieve any pain afterwards. The procedure will also relieve you from pain caused by the infection allowing you to enjoy food without pain from heat, cold, or biting too hard. If you are experiencing pain call us today.
Post-Op
You can expect soreness after a root canal procedure for a few days. You should avoid chewing on the side of your mouth where the procedure was performed so you do not irritate the area and also to ensure that the temporary restorative material properly sets. You may also need to take an antibiotic to treat any remaining infection in your tooth. If you notice an increasing amount of pain or tenderness, a reaction to the medication, or the loss of the temporary restoration (filling) please call us immediately.
With proper care, most teeth that have had endodontic (root canal) treatment can last as long as other natural teeth. Root canals performed by endodontists (root canal specialists) have a 95% success rate. In some cases, however, a tooth that has received endodontic treatment fails to heal. Occasionally, the tooth becomes painful or diseased months or even years after successful treatment.
Why do I need retreatment?
As occasionally happens with any dental or medical procedure, a tooth may not heal as expected after initial treatment for a variety of reasons:
Narrow or curved canals were not treated during the initial procedure.
Complicated canal anatomy went undetected in the first procedure.
The placement of the crown or other restoration was delayed following the endodontic treatment.
The restoration did not prevent salivary contamination to the inside of the tooth.
In other cases, a new problem can jeopardize a tooth that was successfully treated.
For example:
New decay can expose the root canal filling material to bacteria, causing a new infection in the tooth. A loose, cracked or broken crown or filling can expose the tooth to a new infection. A tooth sustains a fracture. Retreatment is performed in two visits and involves the following:
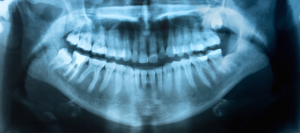
At the initial visit the endodontist will examine the tooth, take x-rays and discuss your treatment options. If you and your endodontist choose retreatment, the retreatment will be scheduled at that time for a future date. At the retreatment appointment the endodontist will administer local anesthetic to numb the tooth. After the tooth is numb, the endodontist will reopen your tooth to gain access to the root canal filling material. In many cases, complex restorative materials (crown, post and core material) must be disassembled and removed to permit access to the root canals. After removing the canal filling, the endodontist can clean the canals and carefully examine the inside of your tooth using a microscope, searching for any additional canals or unusual anatomy that requires treatment. After cleaning the canals, the endodontist will fill and seal the canals and place a temporary filling in the tooth. Post space may also be prepared at this time.
After your endodontist completes retreatment, you will need to return to us right away to have a new crown or other restoration placed on the tooth to protect and restore it to full function. If the canals are unusually narrow or blocked, your endodontist may recommend endodontic surgery.
TMJ is the acronym for temporomandibular joint, which connects your lower jaw (the mandible) to your skull at the temporal bone. This joint controls many jaw functions, like chewing. If the chewing muscles or the joint itself are causing you pain you may have temporamandibular disorder, or TMD. TMD can be caused by stress, continual clenching of the jaw muscles, or teeth grinding.
Some of the symptoms of TMD are:
- Pain when opening or closing mouth
- Trouble chewing
- Jaw becoming stuck open or shut
- Headaches or ear pain
- Clicking or popping sounds when opening your mouth
- Teeth Grinding
Many of these symptoms can often be associated with other health problems, so only a medical professional can tell you if it is due to TMD. Teeth grinding is an especially problematic symptom because it can lead to further problems. Prolonged teeth grinding, or bruxism, can cause enamel to wear off teeth and expose dentin. This material is softer than enamel and more susceptible to decay. Sensitivity to hot and cold food or drink may also develop from excessive teeth grinding.
If you suspect you may have TMD come in for a consultation. We can help diagnose you and provide relief for your symptoms. Pain relievers and hot/cold compresses are short term methods to provide relief for pain symptoms. A night guard can be used to help prevent or lessen the effects of teeth grinding at night. This can lead to a more permanent solution. In very severe cases of TMD surgery may be required, but behavioral treatments to change the way you use your jaw muscles are usually enough to provide relief.